Type 1 vs. Type 2 Diabetes: What You Need to Know
Diabetes is a chronic condition that affects how your body processes glucose, a vital source of energy. While there are different types of diabetes, Type 1 and Type 2 are the most common. Despite sharing some similarities, they differ significantly in their causes, symptoms, and treatment.
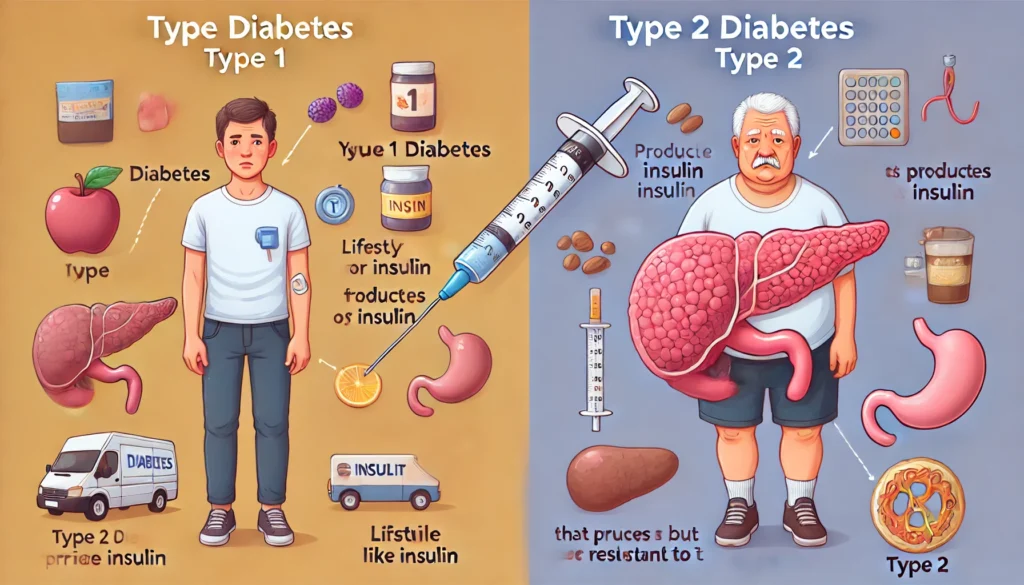
Type 1 Diabetes Type 1 diabetes is an autoimmune condition in which the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. As a result, individuals with Type 1 diabetes produce little to no insulin, a hormone that regulates blood sugar levels. This type of diabetes is often diagnosed in children and young adults but can develop at any age. Its onset is usually sudden, with symptoms such as frequent urination, extreme thirst, weight loss, and fatigue.
People with Type 1 diabetes must take insulin daily to manage their blood sugar levels. Unfortunately, there is currently no way to prevent this form of diabetes, and its cause is not fully understood, though genetics and environmental factors play a role.
Type 2 Diabetes Type 2 diabetes is far more common and is primarily related to insulin resistance. In this case, the body still produces insulin, but the cells do not respond to it effectively. Over time, the pancreas may also produce less insulin, leading to elevated blood sugar levels. This type of diabetes usually develops later in life and is linked to factors like obesity, a sedentary lifestyle, and poor diet, though genetics can also increase the risk.
Unlike Type 1 diabetes, Type 2 can often be managed with lifestyle changes such as improved diet, regular exercise, and weight loss. In some cases, medication or insulin therapy may also be necessary. Early detection and intervention are critical to preventing complications such as heart disease, kidney problems, and nerve damage.
Key Differences The primary difference between Type 1 and Type 2 diabetes lies in the cause and treatment approach. Type 1 is an autoimmune disease requiring lifelong insulin therapy, while Type 2 is more closely associated with lifestyle factors and can sometimes be managed without insulin. Additionally, Type 1 diabetes typically appears earlier in life, whereas Type 2 is more common in adults over 45.
Understanding these differences is crucial for proper diagnosis and management. If you or a loved one experiences symptoms like excessive thirst, unexplained weight loss, or fatigue, it’s important to consult a healthcare provider for appropriate testing and treatment options